1. Introduction
1.1 Smoking
Smoking is a leading cause of preventable death in the United Kingdom (UK). 77,800 deaths were attributable to smoking in England in the latest statistics by National Health Service (NHS) Digital. Passive smoking can be fatal (Jamrozik, 2005), with children most vulnerable. (Cavalcante et al., 2017) In England, 489,300 hospital admissions are attributable to smoking according to NHS Digital’s report ‘Smoking-related ill health and mortality’, with the total annual cost estimated at £2bn, with a further £1.1bn in social care costs according to Public Health England (PHE). The estimated total annual cost of smoking to society in England, including lost productivity and health and social care costs, is £13.9bn as per the ‘Use of E-Cigarettes in Public Places and Workplaces’ report by PHE. Reducing the prevalence of cigarette smoking is therefore a main objective for the government and devolved administrations.
Office for National Statistics (ONS) 2017 statistics on UK adult smoking habits produced in partnership with PHE show that in the UK (including Great Britain and Northern Ireland), 15.1% of people aged 18 years and above smoked cigarettes. This equates to 7.4 million active smokers (14.9% of adults in England, 16.1% for Wales, 16.3% for Scotland and 16.5% in Northern Ireland smoked). In the UK: 17.0% of men smoked compared with 13.3% of women, those aged 25-34 years had the highest proportion of current smokers (19.7%) and 1 in 4 (25.9%) people in routine and manual occupations smoked, compared with just 1 in 10 people (10.2%) in managerial and professional occupations. In Great Britain (includes England, Wales, and Scotland), 60.8% of people aged 16 years and above who currently smoked said they wanted to quit and 59.5% of those who have ever smoked said they had quit.
Similarly, 5.5% of people in 2017 said they currently used an e-cigarette, which equates to approximately 2.8 million adults. Latest estimates on e-cigarette use in Great Britain were: 8.5% of those aged 35-49, 7% of those aged 25-34, 6.8% of those aged 50-59, 6.3% of those aged 16 and over, 4.8% of those aged 16-24 and 4.4% of those aged 60 and over. Women of childbearing age who are current e-cigarette users include 1.1% of Women aged 16-24, 4.7% of Women aged 25-34 and 5.7% of Women aged 35-49.
A 2018 House of Commons report summarises that Tobacco Control Delivery Plan 2017-22 is designed to reduce the prevalence of: 15-year-olds, adults and pregnant women who regularly smoke and to reduce the inequality gap in smoking prevalence. They advise that e-cigarettes could be an aid for smokers attempting to give up conventional cigarettes as per the Tobacco Control Plan for England and the commissioned evidence review. (McNeill et al., 2018) Youth e-cigarette use has increased rapidly, with high prevalence among non-smoking youth. However, the decline in current smoking among 12th graders has accelerated since e-cigarettes have become available. E-cigarette use is largely concentrated among youth who share characteristics with smokers of the pre-vaping era, suggesting e-cigarettes may have replaced cigarette smoking. E-cigarettes may be an important tool for population-level harm reduction, even considering their impact on youth. (Sokol and Feldman, 2021).
Others see e-cigarettes as a health hazard (The National Academies of Sciences, Engineering, and Medicine, 2018) with the United States Surgeon General inviting actions to protect young people from initiating or continuing the use of e-cigarettes. Evidence suggests maternal vaping during pregnancy confers significant cerebrovascular health risk or dysfunction to offspring that persists into adult life. (Burrage et al., 2021) Factors that attract people to e-cigarettes are: a method for smoking cessation, lower price compared to tobacco, better taste/smell, offers similar pleasures associated with smoking and avoiding smoking bans as per literature and ONS report on e-cigarette use in Great Britain. (McKeganey and Dickson, 2017; Toumbis, 2016) These statistics show a worrying up-ward trend in e-cigarette use, for males by age in Great Britain.
1.2 Tobacco Products Directive
The European Union (EU)’s Tobacco Products Directive (TPD Directive 2014/40/EU) provides a legislative framework for e-cigarettes. At the time of writing, the UK has adopted this directive into its legislative framework. “Electronic cigarette” means a product that is intended for inhalation of vapour via a mouthpiece, or any component of that product, including but not limited to cartridges, tanks, or e-liquids. Other terminology includes electronic nicotine delivery systems (ENDS), electronic non-nicotine delivery systems (ENNDS), electronic cigarettes (e-cigarette) and vaping.
1.3 Pharmacy
Community pharmacists and their teams make an important contribution to smoking prevention, and smoking cessation via routine public health promotion, medicines optimisation services and a range of targeted services and interventions specifically designed to stopping smoking as recommended by research and in national guidance (National Institute For Health And Care Excellence, 2018; Public Health England, 2017).
Pharmacies often have extended opening hours, frequently located in comfortable and attractive retail spaces, accessible within 20 minutes’ walk, generally available without appointment and have been shown to provide greater care in areas of highest deprivation. (Adam Todd, Alison Copeland, Andy Husband, Adetayo Kasim, Clare Bambra, 2014) They provide a less intimidating clinical/hospital space for patients, more convenient for people with less access to healthcare. Pharmacists can provide smoking cessation services at reduced cost to the NHS compared to General practitioner (GP) services. (Dalton and Byrne, 2017) Current guidelines (National Institute for health and care excellence, 2018, p. 92) permit contracted workers in primary and community settings to use e-cigarette in such cessation services.
Pharmacy specific research (Erku et al., 2019; Marques Gomes et al., 2016) shows concern about safety and quality of e-cigarettes and related care services provided to patients. A regional English study found that 73% of community pharmacies sold e-cigarettes, mainly to assist smoking cessation. (Marques Gomes et al., 2016) Nicotine levels stated on the packaging were inconsistent with measured values, included toxins (El-Hellani et al., 2018; Goniewicz et al., 2014, 2013; Hitosugi et al., 2019; Williams et al., 2017) and are being manipulated by users to vary the flow rate, dosing, (Buonocore et al., 2017; Farsalinos et al., 2013; Kosmider et al., 2018) and content. (M. Blundell et al., 2018; M. S. Blundell et al., 2018; East et al., 2018; Franck et al., 2016; Hitosugi et al., 2019; Jones et al., 2016; Rennie et al., 2016)
Internationally, the availability and placement of e-cigarettes at the point-of-sale in pharmacies (Wagoner et al., 2018) make them easier to access, though less evidence-based than nicotine replacement therapy (NRT). All forms of NRT made it more likely that a person's attempt to quit smoking would succeed. NRT works with or without additional counselling, and does not need to be prescribed by a doctor. (Hartmann-Boyce et al., 2018) Counselling alongside NRT is an evidence-based strategy. (Bauld et al., 2011; Hartmann-Boyce et al., 2019; Stead et al., 2015) Barnoya et al. (Barnoya et al., 2015) found low access to NRT encouraged smoking disparities in disadvantaged and racially diverse neighbourhoods.
This study seeks to understand how pharmacists (working in registered pharmacy premises) support smoking cessation (primary objective) in a backdrop of growing patient demand, insufficient primary care funding (Oxtoby, 2017), changing patterns of demand, reduced access to GPs and addressing national health inequalities. Pharmacist counselling could be a source of professional information and motivational support towards eliminating tobacco use. A secondary objective was to consider effects of counselling when sales of e-cigarettes are made. This study aligns with the United Nations’ agenda for Sustainable Development Goals 3, targets 3.A.
2. Materials and Methods
Participants and recruitment
We invited pharmacists from 500 pharmacies across England to complete a survey about their experiences of supporting customers who buy e-cigarettes from their pharmacies.
Inclusion Criteria: Community pharmacies that contribute to the National Health Service (NHS) Business Services Authority (BSA) dispensing data. Exclusion Criteria: Community pharmacies that are not NHS contractors, other settings that sell e-cigarette (e.g., vaping shops, hospitals, GP surgeries, walk-in centres).
Addresses were taken from publicly available NHS BSA website (March 2018) to gain a nationally representative sample. We randomly selected 500 pharmacies with contractor code (FAV82 - FYY76), ensuring they were nationally representative with respect to the number of prescription forms (invited sample mean 5184, SD 1965 versus population mean 3564, SD 2692) and number of prescription items dispensed (invited sample mean 10479, SD 4050 versus population mean 7132, SD 5167). This permits comparison with like for like businesses (approximately equal burden of work, similar team size, and similar business complexity) across the country, therefore allowing fair comparison between pharmacies invited to study and the wider pharmacy population.
A single follow-up mail to non-responders was sent in the period December 2018 to April 2019. Respondents were invited to provide self-reported answers in provided self-addressed envelopes.
Questionnaire
The questionnaire composed items relating to demographics, whether e-cigarettes and NRT were sold, if they provided smoking cessation services, describing e-cigarette customers and their purchasing habits, information around point of sale displays for e-cigarettes and NRT, opinions on packaging and labelling of e-cigarette, counselling practices and to describe impact of flavouring (see Appendix A).
Sample size
Sample-size calculation was not done because published estimates of national level sales prevalence of e-cigarettes from community pharmacies are lacking. A convenience sample was used and 500 potential participants were invited.
Data analysis
Analyses were undertaken using SPSS. The results presented are descriptive, presented as proportions and independent sample tests. The opinion scale’s reliability was measured using Cronbach’s alpha. Validity and reliability are closely associated, and a scale cannot be valid unless reliable. Cronbach’s alpha is the most widely used objective measure of reliability and acceptable values range from 0.70 to 0.95.
Mapping
Postcodes of pharmacies were linked with freely available IMD scores, an estimate of the socioeconomic deprivation of the practice population and NHS dispensing data. Results were mapped using ArcGIS® software by Esri. ArcGIS® and created several layers to visualize the data easily: https://portuni.maps.arcgis.com/apps/webappviewer/index.html?id=155d991f38c4487fbb02af826a4ebd60. Responses were mapped alongside the IMD 2015 data (Ranks: every postcode has a rank from 1 which is the most deprived area up to 32,844 which is the least deprived area. Deciles are 1/10th subdivisions and are published alongside ranks to assess relative deprivation).
No Patient and Public Involvement
Patients or public were not involved in this work. This is likely to be done in the future.
Ethics
Favourable institutional ethical approval was received (Science Faculty Ethics Committee Reference Number: SFEC 2018-100; Date Submitted: 27 September 2018). No financial (or similar) benefits were offered to minimise biased responses. STROBE cross sectional reporting guidelines were used.
3. Results and Discussion
Sixty-six responses (13.2%) were received from the duty pharmacist working in the pharmacies that were invited to recruitment. See Table 1 for participant demographic information. Seventeen out of the 66 respondents sold e-cigarette, indicating a sales-prevalence of 25.76% of e-cigarette.
Participant demographic information
| Variables | All Respondent Frequencies (Percentage) (n=66) | Respondents who sell e-cigarette Frequencies (Percentage) (n=17) |
|---|---|---|
| Gender | (2 missing) | |
| Male | 38 (57.6%) | 8 (47.1%) |
| Female | 25 (37.9%) | 9 (52.9%) |
| Preferred not to say | 1 (1.5%) | – |
| Years of registration experience | ||
| 1-2 | 5 (7.6 %) | 1 (5.9%) |
| 3-4 | 6 (9.1 %) | 2 (11.8%) |
| 5-6 | 3 (4.5 %) | 1 (5.9%) |
| 7-8 | 5 (7.6 %) | 2 (11.8%) |
| 9-10 | 6 (9.1 %) | 3 (17.6%) |
| 11-12 | 2 (3.0 %) | 1 (5.9%) |
| 13-14 | 4 (6.1 %) | 1 (5.9%) |
| 15-16 | 1 (1.5 %) | – |
| 17-18 | 2 (3.0 %) | – |
| 19-20 | 3 (4.5 %) | 1 (5.9%) |
| > 20 years | 29 (43.9 %) | 5 (29.4%) |
| Working hours per week | (1 missing) | |
| 16–24 | 3 (4.5%) | 1 (5.9%) |
| 25–34 | 3 (4.5%) | – |
| 35–44 | 38 (57.6%) | 10 (58.8%) |
| 45–54 | 14 (21.2%) | 5 (29.4%) |
| 55+ | 7 (10.6%) | 1 (5.9%) |
| Employer type | (2 missing) | One-Sample Binomial Test p=0.13. |
| Independent pharmacy | 33 (50.0 %) | 3 (17.6%) |
| National chain pharmacy | 30 (45.5 %) | 14 (82.4%) |
| Online pharmacy | 1 (1.5 %) | – |
Onward analysis relates to the 17 respondents who sell e-cigarettes. Three participants were from independent pharmacies whereas 14 (out of the 17) were from national chain pharmacies.
-
a) Availability of NRT and smoking-cessation services.
NRT was available for sale in most pharmacies (n=16, 94.1%), missing (n=1, 5.9%). Cessation services were less frequently available (n=7, 41.2%), or not available (n=9, 52.9%), missing (n=1, 5.9%). While NRT is sold in retail spaces, pharmacy smoking cessation services are often commissioned by local or central government and provided by accredited professionals. Cessation services have been credited with reducing the inequalities in smoking prevalence. (Bauld et al., 2007) There have been recent cuts to public-health funding (Anderson et al., 2018; British Medical Association, 2019; Iacobucci, 2018) and the data reflects that, the choices available to potential quitters are fewer from pharmacy. Absent services may impact communities, as pharmacists are able to make sales but cannot provide motivational support. This leaves customers making decisions based on price, shop-placement, or promotion rather than evidence-based strategies.
-
b) E-cigarette users and their purchases.
Respondents believed that ‘daily smokers’ were most likely to use e-cigarette (n=8, 47.1%), followed by ‘former smokers’ (n=5, 29.4%), missing (n=4, 23.5%). E-cigarette customers were: 25-34-year-old (n=6, 35.3%), 35-44-year-old (n=5, 29.4%), 18-24-year-old (n=2, 11.8%) and older than 65 years of age (n=1, 5.9%), missing (n=2, 11.8%). Accessories were sold daily to 0-2 people (n=13, 76.5%), 3-5 people (n=2, 11.8%) and 6-8 people (n=1, 5.9%), missing (n=1, 5.9%), χ² p=2.454 x 10-4. Some pregnant women (or women of reproductive age) purchased e-cigarettes (n=4, 23.5%), while many do not (n=13, 76.5%), One-Sample Binomial Test, p=0.049.
‘Daily’ and ‘former’ smokers were most likely to use e-cigarettes, which follow national and international trends. 25-44-years-old were frequent consumers, with few older than 65-years. (McKeganey and Dickson, 2017) Accessory sales were small and fits the ‘impulse’ buy strategy employed.
Of those who sell e-cigarettes, 23.5% of pharmacists sold e-cigarettes to pregnant women or women of reproductive age. While the ONS does not collect pregnancy data, it is difficult to confidently quantify the number of pregnant women affected. From this data, a crude estimate of 699 women buy such products from pharmacies in England (11,539 English pharmacies x 0.2576 e-cigarette sellers x 0.235 sales to pregnant women or women of reproductive age). Reasons behind this are documented elsewhere. (Whittington et al., 2018) Pharmacists employ their professional judgement in making sales to an overtly pregnant women, but they have limited guidance and may consider moral and professional liability to guide decisions.
-
c) Point-of-sale placement, pricing, and concentrations.
E-cigarette were placed on top (n=7, 41.2%), exclusively behind (n=5, 29.4%), in front of the counter (n=2, 11.8%) and then in multiple locations within the shop (n=1, 5.9%), missing (n=2, 11.8%). NRT products were placed in multiple locations (n=7, 41.2%), in front (n=5, 29.4%), exclusively behind (n=3, 17.6%) and then on top of the counter (n=1, 5.9%), missing (n=1, 5.9%). This placement reflects ‘impulsive sales’ strategy.
NRT was available for self-selection in most cases (n=14, 82.4%), One-Sample Binomial Test, p=0.004 and not sometimes (n=2, 11.8%), missing (n=1, 5.9%). Staff-assistance was required for NRT sales (n=12, 70.6%) versus otherwise (n=4, 23.5%), missing (n=1, 5.9%). This is a potential barrier to NRT sale.
The cheapest e-cigarettes included Nvee® e-liquid (n=5, 29.41%), Vype® (n=3, 17.65%), Gamucci® (n=1, 5.88%) and generic (n=1, 5.88%), missing (n=7, 41.17%). Ten respondents provided a range of e-cigarettes and prices: Nvee® 18mg/ml, 10ml (£11.99, £14.98, £20), Vype® for 0 mg/ml, 6 mg/ml, or 12mg/ml in variable sizes (£18.99), Infinity® vapour in 50 watts with 50 puffs (£20), Blu Ace® in 50 watts with 50 puffs (£29.99), Vype® Epen x 2 cartridges 18mg/ml (£19.99) and Gamucci® for 2% nicotine and 360 puffs (£10.99).
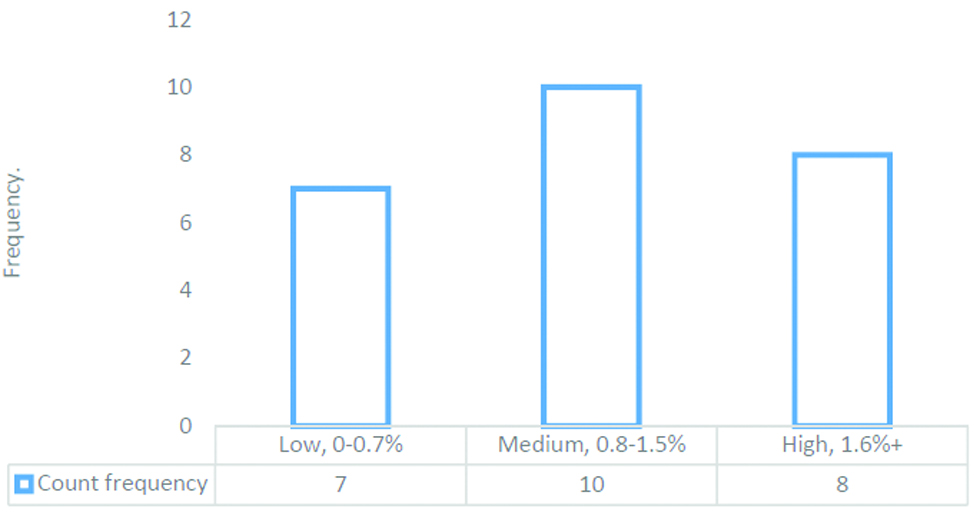
Cheapest NRT Products and prices available for sale from five respondents were Nicorette® gum 2mg unreported pack-size £4.25, Nicorette gum 4mg unreported pack-size £4.99, Nicorette Invisi® patchx7 25mg £7 (“currently half price normally £14”), Nicorette® gum 2mg 105 pieces £10.00, Nicorette® gum 2mg 105 pieces £14.96. Similarly, expensive NRT included Nicorette Qmist® £20.41 1mg/150sprays, Nicorette® gum 4mg 210 pieces £26, Nicorette Qmist® £29.99 1mg 2x150 doses, Nicorette Qmist® £32.24 1mg 2x150 doses, Nicorette® Spray £35.99 1mg 2x150 doses. The narrower range of prices for e-cigarette (£10.99 to £29.99) vs NRT (£4.25 to £35.99) is of note. Thirteen respondents indicated concentration of nicotine cartridges sold in Figure 1, missing (n=4, 23.5%).
Different sales practices between e-cigarette and NRT, suggest economic forces can be influential in ‘if and how’ people quit smoking, especially in deprived areas and with absent cessation services.
Pharmacies place ‘expensive’ items behind the counter for fear of theft. Data shows that requiring staff assistance can be a psychological barrier to access (Trainor and Leavey, 2017) and can be due to decision fatigue (Thompson et al., 2005), anticipated regret/regret aversion (Brewer et al., 2016; Conner et al., 2006) and lack of trust. (Esterberg and Compton, 2005; Ismailov and Leatherdale, 2010; Lucksted et al., 2000; Missen et al., 2013) These practices hinder NRT sale and by its virtue, tacitly promote e-cigarettes as they are placed on top of the counter. (Herrera et al., 2019) The overall range of prices for e-cigarettes was £19 (£10.99 to £29.99) vs £31.74 for NRT (£4.25 to £35.99) potentially make e-cigarettes more affordable, per-unit of equivalent bioavailable nicotine.
Potential visibility of e-cigarettes to children in pharmacies is concerning. Tobacco display bans in England reduced the exposure of children to cigarettes in shops and coincided with a reduction in the proportion of regular child smokers reporting that they bought cigarettes in shops. (Laverty et al., 2019) Similarly, e-cigarettes visibility to children is questionable. This comes in light of e-cigarette maker Juul, who has agreed to settle a lawsuit with a US state that accused the firm of marketing its products to young people. (“Juul to pay $40m in US lawsuit over teen targeting claims,” 2021)
-
d) E-cigarette packaging and labelling.
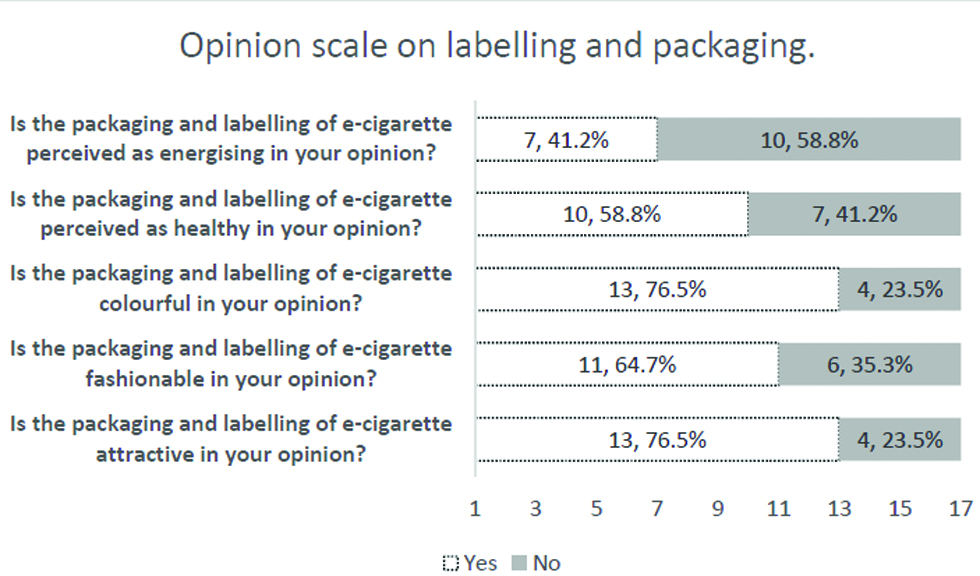
Pharmacists’ experience of handling medicines makes their opinion on packaging valuable. A dichotomous ‘packaging and labelling’ opinion scale was created (Figure 2).
Many labelling and packaging features were attractive (One-Sample Binomial Test, p=0.049), fashionable, colourful (One-Sample Binomial Test, p=0.049), healthy and energising. Such descriptors breach the Directive. Scales’ Cronbach Alpha of 0.780, demonstrates validity. Packaging and labelling were found to be in breach of TPD.
-
e) E-cigarette counselling.
All respondents (n=17, 100%) provided counselling with NRT, (One-Sample Binomial Test p<1 x 10-8). However, less than half (n=8, 47.1%) provide counselling with e-cigarettes, while more than half (n=9, 52.9%) did not. Respondents believed only 29.4% (n=5) of e-cigarette users went on to quit smoking, while 58.8% (n=10) did not, missing (n=2, 11.8%). Counselling was less frequently provided with e-cigarettes. Primarily this could relate to ‘professional bias’s towards e-cigarettes. (Barrett, 2019) As a category, e-cigarettes are licenced as consumer products and they are not traditional regulated items such as ‘medicine’, ‘food’, ‘cosmetic’ or ‘supplements’. Consequently, they may be considered ‘safe’ self-care consumer items, even though nicotine can cause harm. Secondly, pharmacists may not invest in counselling due to lower perceived quit rates, thought this seems to be higher in deprived areas. Equally, these consumers may have lower health literacy, financial ability, may have pre-decided on e-cigarettes use and may not be open to counsel.
-
f) Impact of flavouring.
Eight respondents, describe 22 flavours: 4 cherry, 3 tobacco, 3 mint, 2 menthol, 2 apple, 1 watermelon, 1 mint ice crystal and 1 grape. Respondents reported a better mouth feel/taste (n=5, 29.4%), social impact (n=2, 11.8%) and variety and customisation (n=1, 5.9%), missing (n=9, 52.9%). Flavouring is linked to e-cigarette’s social appeal, especially for children. (Vasiljevic et al., 2016) The TPD, mentions ‘candy’ flavours to be an area of concern - this study finds pharmacies selling cherry, apple, watermelon and grape flavours, which seems questionable professional-practice.
TPD Article 7 prohibits member states from placing on the market of tobacco products with a characterising flavour. However, TPD does not harmonise all aspects of e-cigarettes or refill-containers. As a current/recent EU Member, the UK is free to permit the placing on the market of flavoured products.
-
g) Geospatial analysis.
Respondents were from greater London, Manchester, Brighton, Leeds, Royal Wootton Bassett, Barton le Clay, and Market Weighton, representing a good mix of urban, suburban, and rural communities. Respondent’s IMD decile’s mean was 4.47, SD 2.809 and a SE 0.681, reflecting national average consumers. Dispensing data descriptive statistics (Table 2) show respondents to be representative of invitees.
The data was stratified by decile (See Table 1 in Appendix B by all respondents, Table 2 in appendix B by aggregate deprived (deciles 1-4) versus affluent (deciles 5-9)). An absence of responses from decile 10 was noted.
Deprived versus affluent aggregate data are presented below respectively, because they represent 52.9% versus 47.10% of responding participants who were pharmacists . Nine versus eight pharmacists sold e-cigarettes, NRT was equally available (8 versus 8) in the pharmacies, five versus two pharmacists offered smoking cessation services, eight versus five pharmacists sold e-cigarettes or related accessories daily to 0-2 people.
With respect to customer’s age, an equal number of responding pharmacists came from both deprived and affluent postcodes. However, sub analysis reveals differences: one respondent from deciles one and eight had sold such products to 18 to 24-year-olds. One versus five respondents sold these products to 25 to 36-year-olds in affluent areas. Four versus one respondent sold these products to 35 to 44-year-olds in deprived areas. Daily smokers were less likely to use e-cigarettes in deprived areas (3 versus 5), but never smokers are more likely to use e-cigarettes and be from deprived areas (three versus two).
Three versus two placed e-cigarettes exclusively behind the counter in deprived areas, five versus two placed a cigarette on top of the counter, one versus one placed e-cigarette in front of the counter and only one in an affluent area placed it in multiple locations. Two versus one placed NRT exclusively behind the counter. None vs one place NRT on top of the counter, one versus four placed NRT in front of the counter, and six vs one placed NRT in multiple locations. NRT was available for self-selection equally easily. NRT was most often behind the counter in deprived areas (7 versus 5).
Respondents from deprived areas found the packaging attractive (7 versus 6), fewer found it fashionable (5 versus 6), fewer found it colourful (6 versus 7), and it was equally perceived as healthy (5 versus 5), fewer founded it energising (3 versus 4). Fewer responded sold these items to pregnant women in deprived areas than affluent areas (1 versus 3). Respondents evenly provided counselling (4 versus 4). Those likely to quit smoking using e-cigarette were more likely to be from deprived areas (4 versus 1). Flavour was perceived to impact mouth-feel in deprived areas (3 versus 2). Wider range of concentrations were available in deprived areas (low, medium, and high). More smoking cessation services are provided in deprived area, though commissioning rates are low. (Rosemary Hiscock and Linda Bauld, n.d.) They are likely to have fewer GPs and pharmacies maybe the sole source of healthcare. (Action on smoking and health, 2019) In deprived areas, more flavours and concentrations of e-cigarettes were sold, on the counter-top, with lower access to NRT. (George et al., n.d.) Young-adults use e-cigarette in deprived areas, but established smokers use them less frequently. Affluent young women use e-cigarettes, potentially as cigarettes substitutes, while potentially deprived young women continue to smoke.
Respondent bias assessment based on dispensing volumes.
| NHS Dispensing Monthly (Mar 2018) Statistics | Mean | Standard deviation | ||
|---|---|---|---|---|
| Average England | Respondent | Average England | Respondent | |
| Number of Prescription Forms | 3564 | 5239 | 2692 | 1447 |
| Number of Prescription Items | 7132 | 10143 | 5167 | 2533 |
Strengths and limitations
For the first time, this study reports a national 26% prevalence in e-cigarette sale via community pharmacies in England. Potential breaches of the TPD were identified and geospatial analysis reveals ‘at risk’ groups within the context of deprivation. The discussion on the nature and characteristics of people who are most likely to use e-cigarettes could be based on perceptions of the respondent or facts based on the number of customers they serve which can introduce a degree of bias.
Though we have structured this study robustly, there is a risk of bias. Key limitations of our study are small sample size, low response rate and some missing information. Other limitations may relate to the total survey length, ambiguous questions, and typographical issues.
Potential bias was assessed by dispensing volume (Table 2). Respondents tended to be from busier pharmacies [5239 forms (95% CI 419 to 10100); 1447 items (95% CI 247 to 2650)], which may reflect self-selection bias.
Pharmacies recruited to this study were typical by dispensing volume, including in terms of deprivation of surrounding catchment area. There was a good spread in terms of typology of location (geographically; urban, suburban, rural). Therefore, presented results are robust and credible.
Implications for clinical practice
Findings raise some concerns about the variability in pharmacy offerings, potential TPD breaches and how smoking inequality maybe perpetuated, yet we acknowledge that pharmacies maybe offering help where most-needed. Pharmacists work within their competence and professional standards. (General Pharmaceutical Council, n.d.) but more robust guidance may be required to standardise and benchmark quality practises around the sales of e-cigarettes. It is important to consider the patient population this study may impact. Deprived patients are less likely to see their GP (or not have a GP) and have poor health literacy and outcomes. Community pharmacy maybe their sole source of help and nationally commissioned services via pharmacies could assist in reducing health inequalities. Focusing attention on these people now, can avoid deepening health inequity.
Recommendations
Based on these results, we recommend a unified sales strategy to incorporate a point-of-sale display ban on e-cigarettes from pharmacies, removing candy-flavoured (not mint and menthol) products, preferentially offering NRT at each e-cigarettes sales request and providing dedicated counselling, especially to pregnant women.
3. Conclusions
Pharmacies have ease of access and offer an opportunity for consultation with a registered professional in areas of deprivation, which may or may not be served by vape shops. While a quarter of pharmacies sell e-cigarettes in England, there were variations in offering compared to NRT, sales strategy and counselling levels. In deprived areas, packaging and labelling was potentially in breach of the TPD. No evidence was found that conventional cigarettes smokers are using e-cigarettes as an aid for quitting but find support of non-smokers initiating use. Pharmacists help their patients as best as they can but have limited support. This study makes recommendations to improve practice. Findings of this study are limited by its small sample size and a more robust larger study is required to validate findings. The international research community is encouraged to use this study survey to report their findings.
Acknowledgements
Thank you to the 66-community pharmacy respondent-employees who took the time to provide honest opinions, Louise Vythelingum for helping with study administration and data collection, and Martin Schaefer for his help with ArcGIS publisher requests. This study was funded by the University of Portsmouth.
References
Action on smoking and health. Health Inequalities and Smoking. [WWW Document]. URL. https://ash.org.uk/wp-content/uploads/2019/09/ASH-Briefing_Health-Inequalities.pdf (accessed 9.23.21)..
Adam, Todd; Alison, Copeland; Andy, Husband; Adetayo, Kasim; Clare, Bambra . (2014). The positive pharmacy care law: an area-level analysis of the relationship between community pharmacy distribution, urbanity and social deprivation in England. BMJ Open, 2014 4.
W.J. Anderson, H. Cheeseman, G. Butterworth, (2018). Political priorities and public health services in English local authorities: the case of tobacco control and smoking cessation services. J. Public Health 40 : e269–e274. https://doi.org/10.1093/pubmed/fdx143
J. Barnoya, L. Jin, K.S. Hudmon, M. Schootman, (2015). Nicotine replacement therapy, tobacco products, and electronic cigarettes in pharmacies in St. Louis, Missouri. J. Am. Pharm. Assoc. JAPhA 55 : 405–412. https://doi.org/10.1331/JAPhA.2015.14230
R. Barrett, (2019). Adverse-event management and reporting for electronic cigarettes (e-cigarettes). Eur. J. Hosp. Pharm 26 : 2–3. https://doi.org/10.1136/ejhpharm-2018-001747
L. Bauld, K.A. Boyd, A.H. Briggs, J. Chesterman, J. Ferguson, K. Judge, R. Hiscock, (2011). One-year outcomes and a cost-effectiveness analysis for smokers accessing group-based and pharmacy-led cessation services. Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob 13 : 135–145. https://doi.org/10.1093/ntr/ntq222
L. Bauld, K. Judge, S. Platt, (2007). Assessing the impact of smoking cessation services on reducing health inequalities in England: observational study. Tob. Control 16 : 400–404. https://doi.org/10.1136/tc.2007.021626
M. Blundell, P. Dargan, D. Wood, (2018). A cloud on the horizon-a survey into the use of electronic vaping devices for recreational drug and new psychoactive substance (NPS) administration. QJM Mon. J. Assoc. Physicians 111 : 9–14. https://doi.org/10.1093/qjmed/hcx178
M.S. Blundell, P.I. Dargan, D.M. Wood, (2018). The dark cloud of recreational drugs and vaping. QJM Mon. J. Assoc. Physicians 111 : 145–148. https://doi.org/10.1093/qjmed/hcx049
N.T. Brewer, J.T. DeFrank, M.B. Gilkey, (2016). Anticipated regret and health behavior: A meta-analysis. Health Psychol. Off. J. Div. Health Psychol. Am. Psychol. Assoc 35 : 1264–1275. https://doi.org/10.1037/hea0000294
British Medical Association. Government cuts to smoking cessation services are bad for public health and not cost-effective, says BMA [WWW Document]. URL. https://www.bma.org.uk/news/media-centre/press-releases/2019/march/government-cuts-to-smoking-cessation-services-are-bad-for-public-health-and-not-cost-effective (accessed 12.6.19)..
F. Buonocore, A.C.N. Marques Gomes, S. Nabhani-Gebara, S.J. Barton, G. Calabrese, (2017). Labelling of electronic cigarettes: regulations and current practice. Tob. Control 26 : 46–52. https://doi.org/10.1136/tobaccocontrol-2015-052683
E.N. Burrage, E. Aboaziza, L. Hare, S. Reppert, J. Moore, W.T. Goldsmith, E.E. Kelley, A. Mills, D. Dakhlallah, P.D. Chantler, I.M. Olfert, (2021). Long-term cerebrovascular dysfunction in the offspring from maternal electronic cigarette use during pregnancy. Am. J. Physiol. Heart Circ. Physiol 321 : H339–H352. https://doi.org/10.1152/ajpheart.00206.2021
Cavalcante, D.N. de C.; Sposito, J.C.V.; Crispim B. do, A.; Nascimento A.V., do; Grisolia, A.B. . (2017). Genotoxic and mutagenic effects of passive smoking and urban air pollutants in buccal mucosa cells of children enrolled in public school. Toxicol. Mech. Methods 27 : 346–351. https://doi.org/10.1080/15376516.2017.1288767
M. Conner, M. Conner, T. Sandberg, B. McMillan, A. Higgins, (2006). Role of anticipated regret, intentions and intention stability in adolescent smoking initiation. Br. J. Health Psychol 11 : 85–101. https://doi.org/10.1348/135910705X40997
K. Dalton, S. Byrne, (2017). Role of the pharmacist in reducing healthcare costs: current insights. Integr. Pharm. Res. Pract 6 : 37–46. https://doi.org/10.2147/IPRP.S108047
K. East, L.S. Brose, A. McNeill, H. Cheeseman, D. Arnott, S.C. Hitchman, (2018). Harm perceptions of electronic cigarettes and nicotine: A nationally representative cross-sectional survey of young people in Great Britain. Drug Alcohol Depend 192 : 257–263. https://doi.org/10.1016/j.drugalcdep.2018.08.016
A. El-Hellani, R. Salman, R. El-Hage, S. Talih, N. Malek, R. Baalbaki, N. Karaoghlanian, R. Nakkash, A. Shihadeh, N.A. Saliba, (2018). Nicotine and Carbonyl Emissions From Popular Electronic Cigarette Products: Correlation to Liquid Composition and Design Characteristics. Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob 20 : 215–223. https://doi.org/10.1093/ntr/ntw280
D.A. Erku, C.E. Gartner, J.T. Do, K. Morphett, K.J. Steadman, (2019). Electronic nicotine delivery systems (e-cigarettes) as a smoking cessation aid: A survey among pharmacy staff in Queensland, Australia. Addict. Behav 91 : 227–233. https://doi.org/10.1016/j.addbeh.2018.09.013
M.L. Esterberg, M.T. Compton, (2005). Smoking behavior in persons with a schizophrenia-spectrum disorder: a qualitative investigation of the transtheoretical model. Soc. Sci. Med 61 : 293–303. https://doi.org/10.1016/j.socscimed.2004.11.057
K.E. Farsalinos, G. Romagna, D. Tsiapras, S. Kyrzopoulos, V. Voudris, (2013). Evaluation of electronic cigarette use (vaping) topography and estimation of liquid consumption: implications for research protocol standards definition and for public health authorities’ regulation. Int. J. Environ. Res. Public. Health 10 : 2500–2514. https://doi.org/10.3390/ijerph10062500
C. Franck, K.B. Filion, J. Kimmelman, R. Grad, M.J. Eisenberg, (2016). Ethical considerations of e-cigarette use for tobacco harm reduction. Respir. Res 17 : 53. https://doi.org/10.1186/s12931-016-0370-3
General Pharmaceutical Council. Standards for pharmacy professionals [WWW Document]. URL. https://www.pharmacyregulation.org/standards/standards-for-pharmacy-professionals (accessed 9.23.21)..
E. George, E.G. Consulting, A. Tomlinson, V. Scholey, J.E. Williams, J. Griffiths, (). n.d.. An Independent Review of the Provision of Smoking Cessation Services in Wales 77.
M.L. Goniewicz, P. Hajek, H. McRobbie, (2014). Nicotine content of electronic cigarettes, its release in vapour and its consistency across batches: regulatory implications. Addict. Abingdon Engl 109 : 500–507. https://doi.org/10.1111/add.12410
M.L. Goniewicz, T. Kuma, M. Gawron, J. Knysak, L. Kosmider, (2013). Nicotine levels in electronic cigarettes. Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob 15 : 158–166. https://doi.org/10.1093/ntr/nts103
J. Hartmann-Boyce, S.C. Chepkin, W. Ye, C. Bullen, T. Lancaster, (2018). Nicotine replacement therapy versus control for smoking cessation. Cochrane Database Syst. Rev, https://doi.org/10.1002/14651858.CD000146.pub5
J. Hartmann-Boyce, B. Hong, J. Livingstone-Banks, H. Wheat, T.R. Fanshawe, (2019). Additional behavioural support as an adjunct to pharmacotherapy for smoking cessation. Cochrane Database Syst. Rev, https://doi.org/10.1002/14651858.CD009670.pub4
A.L. Herrera, K.E. Pasch, C.N. Marti, A. Loukas, C. Perry, (2019). Exposure to tobacco marketing in bars predicts subsequent use of multiple tobacco products among non-tobacco-using college students. Tob. Control tobaccocontrol-2019-055195, https://doi.org/10.1136/tobaccocontrol-2019-055195
M. Hitosugi, M. Tojo, M. Kane, N. Shiomi, T. Shimizu, T. Nomiyama, (2019). Criminal mercury vapor poisoning using heated tobacco product. Int. J. Legal Med 133 : 479–481. https://doi.org/10.1007/s00414-018-1923-4
G. Iacobucci, (2018). Stop smoking services: BMJ analysis shows how councils are stubbing them out. BMJ 362, https://doi.org/10.1136/bmj.k3649
R.M. Ismailov, S.T. Leatherdale, (2010). Smoking cessation aids and strategies among former smokers in Canada. Addict. Behav 35 : 282–285. https://doi.org/10.1016/j.addbeh.2009.10.013
K. Jamrozik, (2005). Estimate of deaths attributable to passive smoking among UK adults: database analysis. BMJ 330 : 812. https://doi.org/10.1136/bmj.38370.496632.8F
C.B. Jones, M.L. Hill, D.A. Pardini, M.H. Meier, (2016). Prevalence and correlates of vaping cannabis in a sample of young adults. Psychol. Addict. Behav. J. Soc. Psychol. Addict. Behav 30 : 915–921. https://doi.org/10.1037/adb0000217
Juul to pay $40m in US lawsuit over teen targeting claims, 2021. BBC News..
L. Kosmider, C.F. Kimber, J. Kurek, O. Corcoran, L.E. Dawkins, (2018). Compensatory Puffing With Lower Nicotine Concentration E-liquids Increases Carbonyl Exposure in E-cigarette Aerosols. Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob 20 : 998–1003. https://doi.org/10.1093/ntr/ntx162
A.A. Laverty, E.P. Vamos, C. Millett, K.C.-M. Chang, F.T. Filippidis, N.S. Hopkinson, (2019). Child awareness of and access to cigarettes: impacts of the point-of-sale display ban in England. Tob. Control 28 : 526–531. https://doi.org/10.1136/tobaccocontrol-2018-054511
A. Lucksted, L.B. Dixon, J.B. Sembly, (2000). A Focus Group Pilot Study of Tobacco Smoking Among Psychosocial Rehabilitation Clients. Psychiatr. Serv 51 : 1544–1548. https://doi.org/10.1176/appi.ps.51.12.1544
A.C.N. Marques Gomes, S. Nabhani-Gebara, R. Kayyali, F. Buonocore, G. Calabrese, (2016). Survey of community pharmacists’ perception of electronic cigarettes in London. BMJ Open 6 : e013214. https://doi.org/10.1136/bmjopen-2016-013214
N. McKeganey, T. Dickson, (2017). Why Don’t More Smokers Switch to Using E-Cigarettes: The Views of Confirmed Smokers. Int. J. Environ. Res. Public. Health 14, https://doi.org/10.3390/ijerph14060647
A. McNeill, Brose Leonie, Calder Robert, Bauld Linda, Robson Debbie, (2018). Evidence review of e-cigarettes and heated tobacco products 2018 A report commissioned by Public Health England. London: Public Health England.
A. Memon, J. Barber, E. Rumsby, S. Parker, L. Mohebati, R.O. de Visser, S. Venables, A. Fairhurst, K. Lawson, J. Sundin, (2016). What factors are important in smoking cessation and relapse in women from deprived communities? A qualitative study in Southeast England. Public Health 134 : 39–45. https://doi.org/10.1016/j.puhe.2016.01.014,
R.L. Missen, T. Brannelly, G. Newton-Howes, (2013). Qualitative exploration of family perspectives of smoke-free mental health and addiction services: Smoke-Free Family Involvement. Int. J. Ment. Health Nurs 22 : 294–303. https://doi.org/10.1111/j.1447-0349.2012.00882.x
NICE. Stop smoking interventions and services, National Institute for health and care excellence, guideline [NG92]. Available at:. https://www.nice.org.uk/guidance/ng92 (accessed 12.5.19)..
K. Oxtoby, (2017). Funding cuts result in fewer people accessing smoking cessation services, says charity. Pharm. J, https://doi.org/10.1211/PJ.2017.20203454
Public Health England. Pharmacy: A Way Forward for Public Health Opportunities for action through pharmacy for public health. London: Public Health England.
L.J. Rennie, C. Bazillier-Bruneau, J. Rouëssé, (2016). Harm Reduction or Harm Introduction? Prevalence and Correlates of E-Cigarette Use Among French Adolescents. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med 58 : 440–445. https://doi.org/10.1016/j.jadohealth.2015.12.013
Rosemary, Hiscock; Linda, Bauld . (). n.d.. Stop Smoking Services and Health Inequalities. National Centre for Smoking Cessation and Training (NCSCT),
N.A. Sokol, J.M. Feldman, (2021). High school seniors who used e-cigarettes may have otherwise been cigarette smokers: Evidence from Monitoring the Future (United States, 2009-2018). Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob. ntab102, https://doi.org/10.1093/ntr/ntab102
L.F. Stead, P. Koilpillai, T. Lancaster, (2015). Additional behavioural support as an adjunct to pharmacotherapy for smoking cessation. Cochrane Database Syst. Rev, https://doi.org/10.1002/14651858.CD009670.pub3
The National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-Cigarettes, https://doi.org/10.17226/24952
D.V. Thompson, R.W. Hamilton, R.T. Rust, (2005). Feature Fatigue: When Product Capabilities Become Too Much of a Good Thing. J. Mark. Res 42 : 431–442. https://doi.org/10.1509/jmkr.2005.42.4.431
M. Toumbis, (2016). Electronic Nicotine Delivery Systems A review for clinicians. Pneumon 29,
K. Trainor, G. Leavey, (2017). Barriers and Facilitators to Smoking Cessation Among People With Severe Mental Illness: A Critical Appraisal of Qualitative Studies. Nicotine Tob. Res 19 : 14–23. https://doi.org/10.1093/ntr/ntw183
M. Vasiljevic, D.C. Petrescu, T.M. Marteau, (2016). Impact of advertisements promoting candy-like flavoured e-cigarettes on appeal of tobacco smoking among children: an experimental study. Tob. Control 25 : e107–e112. https://doi.org/10.1136/tobaccocontrol-2015-052593
K.G. Wagoner, E.Y. Song, J.L. King, K.L. Egan, B. Debinski, M. Wolfson, J. Spangler, E.L. Sutfin, (2018). Availability and Placement of Electronic Nicotine Delivery Systems at the Point-of-Sale. Nicotine Tob. Res. Off. J. Soc. Res. Nicotine Tob 20 : 1020–1024. https://doi.org/10.1093/ntr/ntx207
J.R. Whittington, P.M. Simmons, A.M. Phillips, S.K. Gammill, R. Cen, E.F. Magann, V.M. Cardenas, (2018). The Use of Electronic Cigarettes in Pregnancy: A Review of the Literature. Obstet. Gynecol. Surv 73 : 544–549. https://doi.org/10.1097/OGX.0000000000000595
M. Williams, K. Bozhilov, S. Ghai, P. Talbot, (2017). Elements including metals in the atomizer and aerosol of disposable electronic cigarettes and electronic hookahs. PloS One 12 : e0175430. https://doi.org/10.1371/journal.pone.0175430